Emma writes...
Thoughts, resources and comment from the NHD Editor.
Dysphagia and the IDDSI framework
Dysphagia is the term used when someone has swallowing difficulties.[1]
This can be as a result of an underlying condition, for example, a stroke or other neurological conditions, cleft lip and/or palate, head or neck cancer, or reflux. It can also be a side effect of some medications and treatments.
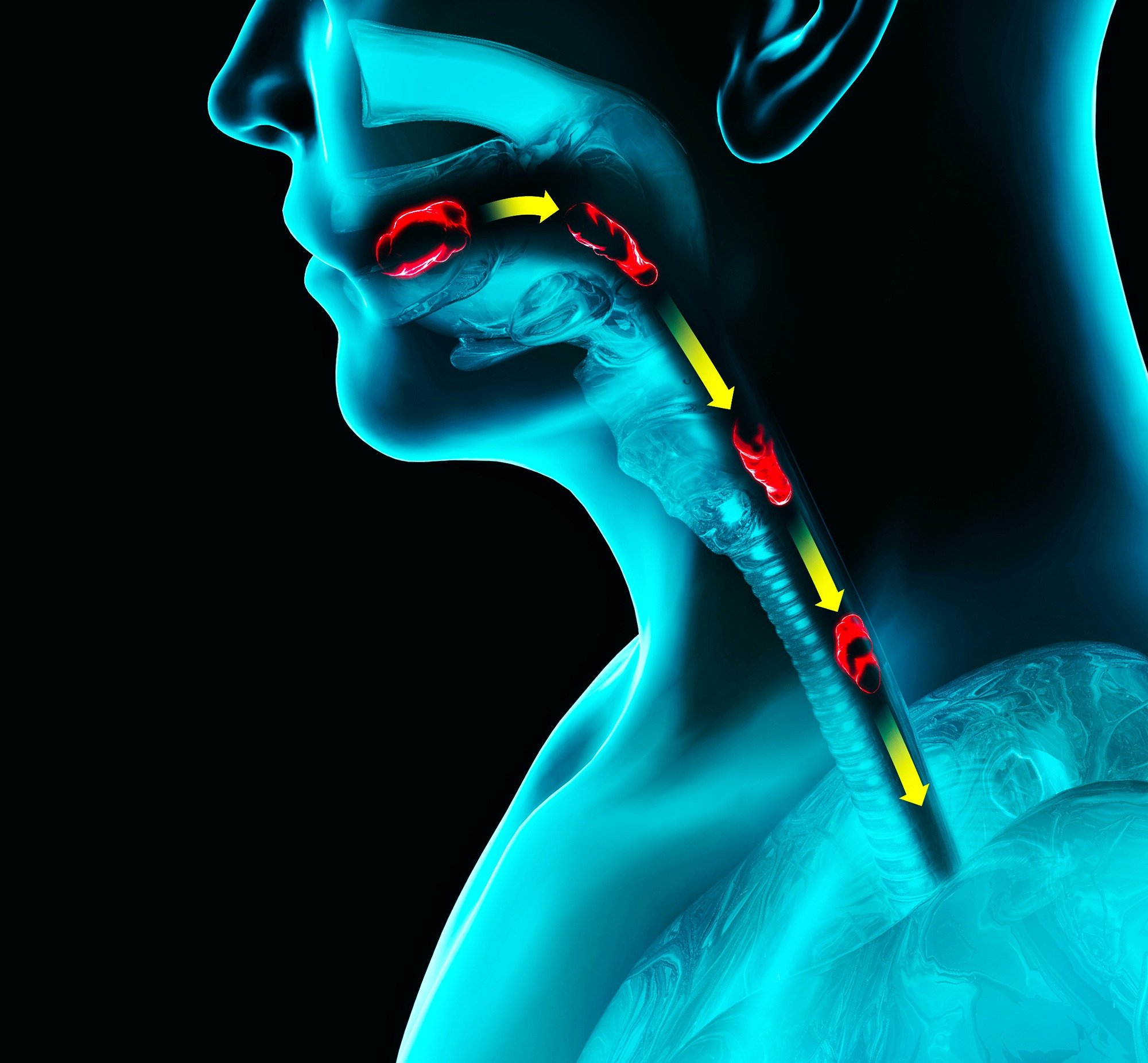
When we eat and drink there are several moving parts and a complex physical and neurological process takes place. It involves the co-ordination of the muscles and nerves in the mouth, throat and oesophagus. When this process is disrupted in some way, symptoms can range from subtle changes to obvious difficulties during this vital part of the eating and drinking experience.
Symptoms can vary from person to person, and will depend on the type of dysphagia they have.
Oropharyngeal dysphagia – where swallowing difficulties are caused by problems in the mouth or throat.
Oesophageal dysphagia – where difficulties are due to oesophageal problems.
If the muscles used for swallowing are not working properly, one or more of the following may occur:[2]
Difficulty keeping food or liquids in the mouth
Difficulty biting or chewing
Difficulty moving and controlling food and liquids in the mouth
Difficulty moving food to the back of the mouth
Bits of food getting left in the mouth
Food or liquids getting stuck in the throat
Food or liquid going into the windpipe (aspiration), causing coughing, choking, chest infections and pneumonia
The impact of dysphagia
There are some significant clinical consequences of dysphagia which have a huge impact on a person’s wellbeing and quality of life (QOL).
These include:[3]
Aspiration – Over 50% of patients with dysphagia experience aspiration. Increased risk of aspiration is liked with chest infections, aspiration pneumonia and increased incidence of mortality.
Dehydration – Between 58-75% of patients experience dehydration.
Malnutrition – There is a correlation between the severity of dysphagia and the incidence of malnutrition.
Length of hospital stay – Patients with dysphagia have a 40% increase in length of hospital stay.
Reduced QOL – In over 50% of head and neck cancer patients, it has been reported that there is a reduction in QOL due to dysphagia.
Appropriate and effective management of dysphagia is vital to ensure that the risks of malnutrition, dehydration and aspiration are addressed and minimised where possible.
Management of dysphagia
There is a range of approaches to manage dysphagia that aim to keep the person safe, support nutritional intake, support rehabilitation where possible, or provide compensation strategies if required.
Speech and language therapists play a key role in the assessment and management of swallowing difficulties. Alongside this, dietitian support with the assessment of dietary requirements ensures nutritional adequacy within the dysphagia management strategy.
Typical management strategies include: [2,3,5-8]
Texture modified diet – Altering the texture of the food can support the preparation of food for swallowing, for example, where there are challenges with chewing or there is an oesophageal limitation such as a narrowing or blockage.
Altered fluid consistency – Liquids can be difficult to control in the mouth and as they pass through the oesophagus to the stomach. They move fast, which can be a safety concern. Thickening drinks means that they are more viscous and slower moving throughout this process. It allows effective swallowing, giving time for the trachea to close, protecting the airway and reducing the risk of aspiration (liquid penetrating the lungs).
Seating and posture techniques / supportive equipment – advice on sitting or being positioned in an upright position during and after eating and drinking is often provided for safety and comfort. Supportive equipment such as specialist dysphagia cups and cutlery may be used to manage the amount of food or drink administered per mouthful. These may be used in conjunction with support from a carer if the person experiences difficulties when feeding themselves.
Swallowing exercises – techniques to strengthen muscles in the mouth and throat which can support rehabilitation and prevent further swallowing problems.
The IDDSI framework
The International Dysphagia Diet Standardisation Initiative[4] (IDDSI) framework has been part of our world for several years now and has provided the standard for defining dysphagia diet and fluid terminology - how we describe the characteristics of food and drinks.
It also provides testing methods to determine whether food and drinks meet the IDDSI standard.
Adopted in many countries around the world, IDDSI really has become the global language for the dysphagia diet.
Why did we need IDDSI?
Before IDDSI was a thing, there were multiple food and drink descriptors in use in various countries.
Using descriptions of food and drinks such as ‘puree’, ‘minced’, ‘mashed’, ‘syrup’ or ‘custard thick were a typical part of dietary texture and consistency modification, a very common management strategy for dysphagia.
Whilst these were developed with the best intentions to keep those experiencing dysphagia safe – aiming to reduce the risk of choking, aspiration or death, they were confusing and open to misinterpretation. They also varied from location to location, meaning there was no consistent method in place. All factors which contribute to the increased risk of morbidity and death.
What IDDSI is and isn’t
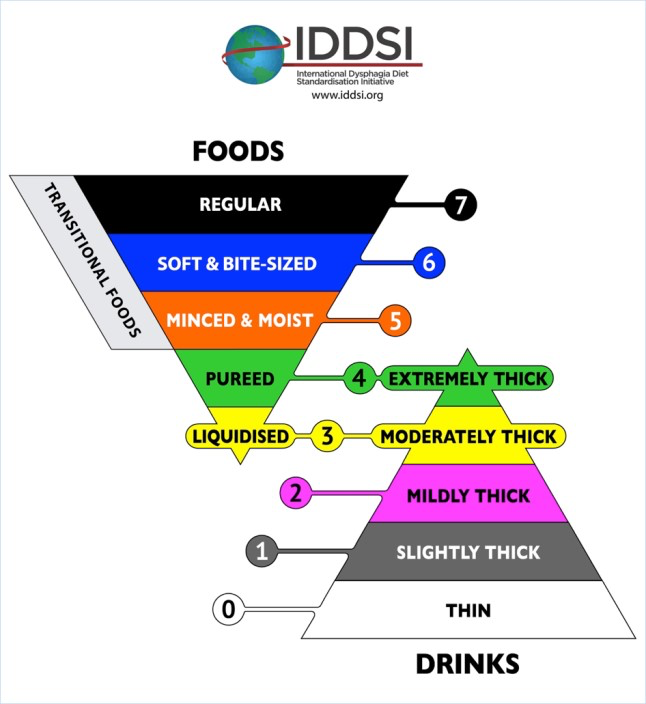
It’s a standard approach to describing the characteristics of food and drinks from the perspective of a person with dysphagia. That is, it is a way to classify a food or a drink into one of eight categories:[9]
Level 0: Thin drinks
Level 1: Slightly thick drinks
Level 2: Mildly thick drinks
Level 3: Moderately thick drinks and pureed foods
Level 4: Extremely thick drinks and minced foods
Level 5: Soft foods
Level 6: Soft and bite-sized foods
Level 7: Regular texture foods
This system not only allows consistency in the description of food and drinks, but it also includes methods for testing to 'confirm the flow or textural characteristics of a particular product at the time of testing'.[9]
The testing is designed to support confirmation of which classification a food and drink falls into, which may be consumed by a person who has swallowing difficulties.
You can read more about IDDSI testing methods here.
Testing foods and drinks requires competency and should be completed by a trained individual. IDDSI recommend that testing should only be conducted on foods and drinks under their intended serving conditions, that is, at the temperature and consistency that the person with swallowing difficulties will be consuming them.
It can be challenging to classify some foods and drinks as they may alter in texture and consistency under shifting conditions, for example, frozen foods when defrosting or foods when heated from chilled or ambient temperatures.
The standard only describes food and drinks; it is not intended to be used to select what level(s) of food and drinks are appropriate for a person. Choosing foods from certain IDDSI levels may play a role in alleviating symptoms,[9] but it remains the responsibility of the healthcare professional who’s managing the person’s needs to ensure that any recommended food and drinks are safe, appropriate and manageable for the person to consume.
Want to know more about IDDSI?
Here’s how you can get to know IDDSI better or refresh your existing knowledge:
Visit the website - Home - IDDSI It holds a wealth of information and free resources in multiple languages. A great hub for any IDDSI related stuff!
Sign up for IDDSI E-bite - IDDSI : Sign Up to Stay in Touch Receive regular updates from IDDSI about any new developments, resources and events. Sign up for free.
Keep an eye out for events – Events - IDDSI
A valuable part of any healthcare professional’s CPD, events are a great way to update and learn, and network with other people in your field.
Coming up soon! - UK IDDSI Academy Pilot 2025 September 16th, 2025. St Michael’s Centre, Bristol, UK
A multidisciplinary pilot course consists of two parts: a mandatory online learning component (to be completed prior to in-person training) and a full day of in-person training on the IDDSI framework, testing methods, practical application, and hands-on practice with faculty feedback. The advanced training of the IDDSI Academy pilot will be exclusively conducted by IDDSI Global, with teaching materials provided by subject matter experts. Discover more about this event here - Bristol 2025 - Events - IDDSICheck out the UK IDDSI Reference Group - United Kingdom - IDDSI More updates and information from UK based experts in dysphagia management and IDDSI.

Emma has been a Registered Dietitian for over 18 years and has experience in adult and paediatric dietetics. She has been the Editor of NHD for nine years, steering the editorial content and supporting the production process.
Emma currently works in industry.
Emma Coates, RD
References
NHS (2023) Dysphagia (swallowing problems). Dysphagia (swallowing problems) - NHS
NHS Hull University Teaching Hospitals NHS Trust (2024) Dysphagia (Swallowing problems). Dysphagia (Swallowing problems) | Hull University Teaching Hospitals NHS Trust
Holdoway, A. & Smith, A. (2019) Dysphagia A Healthcare Professionals Fact Sheet. Dysphagia A HEALTHCARE PROFESSIONAL FACT SHEET
The International Dysphagia Diet Standardisation Initiative (IDDSI) (2025) About Us. About Us - IDDSI
Worcester Acute Hospitals NHS Trust (2022) Patient Information – Swallow Exercises. worcsacute.nhs.uk/documents/documents/patient-information-leaflets-a-z/swallowing-exercises//?layout=file
Royal Berkshire NHD Foundation Trust (2023) Swallowing exercises:
HAWK exercise (base of tongue strengthening). hawk-exercise-base-of-tongue-strengthening-_jul23.pdf
St George’s University Hospitals NHD Foundation Trust (2023) Swallow Rehabilitation. SLT_SWR.pdf
The International Dysphagia Diet Standardisation Initiative (IDDSI) (2025) Framework – The IDDSI Framework (the standard) The IDDSI Standard - Standards - IDDSI
The International Dysphagia Diet Standardisation Initiative (IDDSI) (2025) Overview. Overview - About Us - IDDSI

