NHD Paediatric Hub
Blended diet: nutrition support at home
There has been debate around the use of blended diets for enterally-fed patients recently. Blended diet is growing in popularity and with the right support can be beneficial for families and the young person requiring nutrition support at home.
The prevalence of children who are classed as being home enteral tube fed has grown significantly in recent years (1). This is partially due to improved life expectancy within this patient group.
Enteral tube feeding can be required for a variety of reasons but primarily because the child is unable to meet their nutritional requirements orally. Traditionally these children would be given a milk-based commercial formula that is nutritionally complete. This can be hung for many hours and can be given as either bolus or continuous feed depending on tolerance and preference.
It has been well recognised that children who are tube-fed often have an increase in GI symptoms around tolerance of feed (2). Symptoms can include reflux, nausea, poor stooling (constipation or loose stools) and general periods of irritability.

WHAT IS BLENDED DIET?
Blended diet has grown in popularity over the last decade and there is now a growing number of parents/carers requesting blended diet as a means to feed their tube-fed child in place of commercial formula. Blended diet can be defined as giving solid food blended and mixed with water or any other liquid through the feeding device of a patient requiring tube feeding. Blended diet can be given as a sole source of nutrition or as an adjunct to commercial formulae (2).
WHAT ARE THE BENEFITS?
Benefits of blended diet have been well documented within the literature (2-4). There are reports of improvements around GI symptoms, such as reflux, constipation and loose stooling, often with an associated reduction in the use of medicines to treat these conditions. There are psychological benefits too, both for the parents/carers and for patients receiving a blended diet. A positive impact on the gut microbiome has been reported (2), which will be linked to improved GI symptoms and there is a feeling of improved wellbeing within this patient group.
ANY AREAS OF CONCERN?
Blended diet however also comes with risks and areas of concern. These include tube blockage, food hygiene, questions regarding nutritional adequacy of the diet, and medication absorption.

CASE STUDY
H is a four-year-old boy with cerebral palsy. He has been tube fed since infancy due to an unsafe swallow. H had a button gastrostomy placed around two years ago and is well-established on his feed plan.
H has issues with reflux and vomiting – he vomits every morning after his overnight feed and is often uncomfortable post-feeds throughout the day. He has maximum dose proton pump inhibitors but they have little impact. H is constipated and requires additional medication to help him stool, this adds to the volume required daily, which, in turn, makes his reflux worse.
H is fed overnight with continuous and daytime boluses; however, his parents take turns staying up at night to ensure he doesn’t vomit.
H is currently on a whole protein feed (1.5kcal/ml). He has tried peptide and milk-free feeds in the past with no improvement in symptoms. There has been discussion about Lap Nissens Fundoplication or jejunal feeding; however, the parents have requested we trial blended diet prior to this. H's weight gain has been poor and he had crossed over two centiles. Surgeons and wider MDT are happy to support blended diet.
H's parents have requested we trial blended diet... Surgeons and wider MDT are happy to support blended diet in his case.
CONSIDERATIONS ON INTRODUCING BLENDED DIET
Before a child is started on blended diet, the family, paediatrician and a dietitian (with experience of blended diet) should meet and have a discussion with the parents. Within this meeting, the family’s expectations should be discussed and a risk assessment carried out. Healthcare professionals should highlight the benefits and potential risks of blended diet and a joint decision made as to what is best for the patient (5). For H in our case study, the decision was made to start blended diet; therefore, more in depth discussions took place with the dietitian.
POTENTIAL RISKS DISCUSSED
The BDA practice Toolkit was launched in 2021 and provides detailed information regarding commencing blended diet, along with an example blended diet competency tool (5). The three main areas of potential risk are tube blockage, nutritional adequacy of blends and food hygiene risk. each of these should be highlighted and discussed in turn with parents/carers.
1. Tube blockage
The consistency of blends should be clearly explained to parents/carers to minimise this risk. The International Dysphagia Diet Standardisation Initiative (IDDSI) provides a framework explaining textures of food and liquids and can be a useful starting resource to explain the consistency of blends. Level 4 is the blend usually required to provide adequate consistency and examples of this can be given. If parents find the blend too stiff to administer then additional liquid should be added. Blended food can be given throughout the day as boluses and will require to be increased in volume over time.
Families starting on their blended diet journey will require a high-power blender to ensure meals are blended smooth enough to prevent tube blockage. There are a variety of blenders available and the higher the power the smoother the blender should be able to get the food, making it safer and reducing the risk of tube blockage.
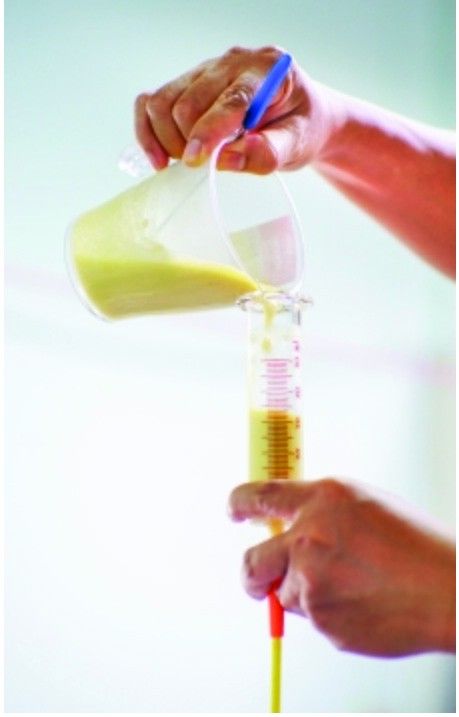
It is recommended that blends are given via a 60ml syringe and depending on the child and tolerance they may need to build up to this volume. Typically, children will take two to four syringes for meals depending on age and tolerance. Thicker blends should be given in 5-10ml increments, which is felt to be a similar rate to children chewing and swallowing a meal. The full volume of blends should be administered in around 20 minutes. It is not recommended to give blended diet via feeding pump.
2. Nutritional adequacy of blends
When feeding with a commercial formula, dietitians know exactly how much macro- and micronutrients a child is receiving. As commercial formula is decreased and real food diets are increased, this becomes more difficult to know. Another concern is that as blends are made more dilute to ensure they are able to pass through the feeding tube, the calories become reduced. Parents should be given advice from a paediatric dietitian who should use their knowledge and skills to ensure blended meals will meet the nutritional needs of the tube-fed individual. The amount of support a family requires will vary depending on their own knowledge, and support should be specific to their needs.
3. Food hygiene
Blended diet is not sterile and, therefore, can cause infection or food poisoning. Care should be given to discuss food hygiene recommendations, including safe cooking, cooling and storage of blends, to minimise risk.
CASE STUDY CONTINUED...
The above risks were discussed with H’s parents along with a plan for feeding when/if H would be admitted to hospital. H and parents then commenced his blended diet journey and started to increase the volumes of blends by introducing one meal at a time and decreasing the commercial formula used. Within several weeks, his parents felt they had a happier boy who appeared more settled. H continued to vomit post his overnight feed, but his tolerance of daytime blends in place of commercial formula was better. The family then made the decision to stop the overnight feed and increase the blends during the day. At this stage, H was on three meals and two to three snacks daily.
Six months post starting blended diet, H was reviewed by the MDT, who had suggested jejunal feeding or fundoplication. The parents described H as a different boy: he was happier and more comfortable during the day and he required practically no venting of his gastrostomy. H had stopped vomiting in the morning and his proton pump inhibitor had now been stopped. Stooling was better and the parents described this as normal. He was no longer on any laxatives as routine.
The parents reported H appeared brighter and they felt his skin and eyes sparkled more and he had better hair growth.
H's parents also reported a great amount of pleasure in being able to feed H normal food, something which they had never been able to do, and felt both H and themselves benefited from him taking part in normal family meal times. H’s weight had improved and he had started moving back up through the centiles. The decision was made by his parents and the MDT that he should continue on blended diet and that there was no justification for any further surgical procedures.
CONCLUSION
H’s case demonstrates a very positive outcome for a complex child with multiple medical issues. His family were able to avoid surgery and the complications that go alongside a general anaesthetic. Blended diet is growing in popularity and with the right support can be beneficial for families and the young person both in terms of reducing the medical burden of care and by providing a sense of normalcy and control for parents caring for a child with medical complexity.

Instagram: kidsnutritionrd
Website: www.kids-nutrition.com
Hazel Duncan, RD
Paediatric Dietitian, Kids Nutrition
References
- Glasson EJ, Wong K, Leonard H, Forbes D, Ravikumara M, Mews C. Evolving trends of gastrostomy insertion within a paediatric population. Journal of Paediatric Gastroenterology & nutrition. 2018: 67: e89-e94
- McCormack S, Patel K & Smith C. Blended diet for enteral tube feeding in young people: A systematic review of the benefits and complications. Journal of Human Nutrition & Dietetics. 2023; 1-16
- Soscia J, Adams S, Cohen E, Moore C, Friedman JN, Gallagher K, Marcon M, Nicholas D, Weiser N & Orkin J. The parental experience and perceptions of blenderized tube feeding for children with medical complexity. Paediatrics & Child Heath. 2021; 462-469
- Koglmeier J, Assecaira I, Banci E, De Koning B, Haiden N, Indrio F, Kastelijn W, Kennedy Dm Luque V, Norsa L, Verduci E & Sugar A. The use of Blended diets in Children with Enteral Feeding tubes: a Joint Position Paper of the ESPGHAN Committees of Allie dHealth Professionals and Nutrition. Journal of Paediatric Gastroenterology and Nutirtion. 2023; 76(1) 109-117
- Durma S, Kennedy A, Kennedy D, Stanley R, Donohoe S, Thomas S & Constable L. Practice Toolkit: The Use of Blended Diet with Enteral Feeding Tubes. [online]
