PLANT-BASED PARENTING pg 10
Aqsa Mahmood, ANutr
- The Vegan Society. https://www.vegansociety.com/news/media/statistics
- Find out how many vegans there are in Great Britain. The Vegan Society. 17 May, 2016. https://www.vegansociety.com/whats-new/news/find-out-how-many-vegans-there-are-great-britain
- Definition of veganism. The Vegan Society. https://www.vegansociety.com/go-vegan/definition-veganism
- Children - British Nutrition Foundation. https://www.nutrition.org.uk/healthyliving/lifestages/children.html?start=5
- Healthy Eating - British Dietetic Association. https://www.bda.uk.com/resource/healthy-eating.html
- The vegan diet - NHS. https://www.nhs.uk/live-well/eat-well/the-vegan-diet/
- Vegetarian, vegan and plant-based diet - British Dietetic Association. https://www.bda.uk.com/resource/vegetarian-vegan-plant-based-diet.html
- Paediatric Nutrition Handbook (2009)
- Vitamins and minerals - Iron – NHS. https://www.nhs.uk/conditions/vitamins-and-minerals/iron/
- Vitamins and minerals - Iodine - NHS. https://www.nhs.uk/conditions/vitamins-and-minerals/iodine
- Iodine Food fact Sheet - British Dietetic Association. https://www.bda.uk.com/resource/iodine.html
- The growth and development of vegan children - Sanders (1992). https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-277X.1992.tb00129.x
- Vitamin B12 or folate deficiency anaemia. https://www.nhs.uk/conditions/vitamin-b12-or-folate-deficiency-anaemia/
- Vitamins and minerals - Vitamin D - NHS. https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/
- How to get more fibre into your diet - NHS. https://www.nhs.uk/live-well/eat-well/how-to-get-more-fibre-into-your-diet/
CYSTIC FIBROSIS IN CHILDREN: NUTRITIONAL MANAGEMENT pg 13
Barira Saad RD, PNDS
- https://www.cysticfibrosis.org.uk/sites/default/files/2020-12/2019%20Registry%20Annual%20Data%20report_Sep%202020.pdf
- https://www.cysticfibrosis.org.uk/what-is-cystic-fibrosis/what-causes-cystic-fibrosis
- Cystic Fibrosis Trust. Cystic Fibrosis: Strength in Numbers. UK Cystic Fibrosis Registry. Annual Report 2017. www.cysticfibrosis.org.uk. Accessed 31 December 2018
- Castellani C, Massie J, Sontag M et al. Newborn screening for cystic fibrosis. Lancet Respir Med, 2016, 4 656-661
- Dijk FN, Fitzgerald DA. The impact of newborn screening and earlier intervention on the clinical course of cystic fibrosis. Paediatr Respir Rev, 2012, 13 220-225
- Dijk FN, McKay K, Barzi F et al. Improved survival in cystic fibrosis patients diagnosed by newborn screening compared to historical cohort from the same centre. Arch Dis Child, 2011, 96 1118-1123
- Coffey MJ, Whitaker V, Gentin N et al. Differences in outcomes between early and late diagnosis of cystic fibrosis in the newborn screening era. J Pediatr, 2017, 181 137-145.e1
- Ren CL, Borowitz DS, Gonska T et al. Cystic fibrosis transmembrane conductance regulator related metabolic syndrome, and CF screen positive, inconclusive diagnosis. J Pediatr, 2017, 181s S45-S51.e1
- Vandenbranden SL, McMullen A, Schechter MS et al. Lung function decline from adolescence to young adulthood in cystic fibrosis. Pediatr Pulmonol, 2012, 47(2) 135-143
- Lai HJ, Shoff SM, Farrell PM. Recovery of birth weight z score within 2 years of diagnosis is positively associated with pulmonary status at 6 years of age in children with cystic fibrosis. Pediatrics, 2009, 123(2) 714-722
- Stallings VA, Stark LJ, Robinson KA et al. Evidence‐based practice recommendations for nutrition‐related management of children and adults with cystic fibrosis and pancreatic insufficiency: results of a systematic review. J Am Diet Assoc, 2008, 108(5) 832-839
- McPhail GL, Acton JD, Fenchel MC et al. Improvements in lung function outcomes in children with cystic fibrosis are associated with better nutrition, fewer chronic Pseudomonas aeruginosa infections, and dornase alfa use. J Pediatr, 2008, 153(6) 752-757
- Sharma R, Florea VG, Bolger AP et al. Wasting as an independent predictor of mortality in patients with cystic fibrosis. Thorax, 2001, 56(10) 746-750
- Beker LT, Russek‐Cohen E, Fink RJ. Stature as a prognostic factor in cystic fibrosis survival. J Am Diet Assoc, 2001, 101(4) 438-442
- Pedreira CC, Robert RGD, Dalton V et al. Association of body composition and lung function in children with cystic fibrosis. Pediatr Pulmonol, 2005, 39(3) 276-280
- National Institute for Health and Care Excellence. Gastro‐Oesophageal Reflux Disease in Children and Young People: Diagnosis and Management. NICE Guideline NG1, January 2015. www. nice.org.uk. Accessed 31 December 2018
- Coates A, Crofton P, Marshall T. Evaluation of salt supplementation in CF infants. J Cyst Fibros, 2009, 8(6) 382-385
- Neumark‐Sztainer D, Story M, Falkner NH et al. Disordered eating among adolescents with chronic illness and disability: the role of family and other social factors. Arch Pediatr Adolesc Med, 1998, 152(9) 871-878
- Shearer JE, Bryon M. The nature and prevalence of eating disorders and eating disturbance in adolescents with cystic fibrosis. J R Soc Med, 2004, 97(4) 36-42
- Maqbool A, Schall JI, Gallagher PR, Zemel BS, Strandvik B, Stallings V. Relation between dietary fat intake type and serum fatty acid status in children with cystic fibrosis. J Pediatr Gastroenterol Nutr. 2012; 55(5): 605-11
- Smyth RL, Rayner O. Oral calorie supplements for cystic fibrosis. Cochrane database Syst Rev. 2014; 11:CD000406
- White H, Morton AM, Peckham DG, Conway SP. Dietary intakes in adult patients with cystic fibrosis – do they achieve guidelines? J Cyst Fibros. 2004; 3(1): 1-7
- Shepherd RW, Holt TL, Cleghorn G, Ward LC, Isles A, Francis P. Short-term nutritional supplementation during management of pulmonary exacerbations in cystic fibrosis: a controlled study, including effects of protein turnover. Am J Clin Nutr. 1988; 48(2): 235-9
- Rettammel AL, Marcus MS, Farrell PM, Sondel SA, Koscik RE, Mischler EH. Oral supplementation with a high-fat, high-energy product improves nutritional status and alters serum lipids in patients with cystic fibrosis. J Am Diet Assoc. 1995; 95(4): 454-9
- Skypala IJ, Ashworth FA, Hodson ME, Leonard CH, Knox A, Hiller EJ et al. Oral nutritional supplements promote significant weight gain in cystic fibrosis patients. J Hum Nutr Diet. 1998; 11(2): 95-104
- Steinkamp G, Demmelmair H, Rühl-Bagheri I, von der Hardt H, Koletzko B. Energy supplements rich in linoleic acid improve body weight and essential fatty acid status of cystic fibrosis patients. J Pediatr Gastroenterol Nutr. 2000; 31(4): 418-23.
- https://www.cysticfibrosis.org.uk/sites/default/files/2020-12/Nutritional%20Management%20of%20cystic%20fibrosis%20Sep%2016.pdf
- Truby H, Cowlishaw P, O’Neil C, Wainwright C. The long-term efficacy of gastrostomy feeding in children with cystic fibrosis on anthropometric markers of nutritional status and pulmonary function. Open Respir Med J. 2009 Jan; 3:112-5
- Best C, Brearley A, Gaillard P, Regelmann W, Billings J, Dunitz J et al. A pre-post retrospective study of patients with cystic fibrosis and gastrostomy tubes. J Pediatr Gastroenterol Nutr. 2011; 53(4): 453-8
- Bradley GM, Carson KA, Leonard AR, Mogayzel PJ, Oliva-Hemker M. Nutritional outcomes following gastrostomy in children with cystic fibrosis. Pediatr Pulmonol 2012; 47(8): 743-8
- Walker SA, Gozal D. Pulmonary function correlates in the prediction of long-term weight gain in cystic fibrosis patients with gastrostomy tube feedings. J Pediatr Gastroenterol Nutr. 1998; 27(1): 53-6
- Morton A, Wolfe S. Enteral tube feeding for cystic fibrosis. Cochrane database Syst Rev. 2015; 4: CD001198
- Kalnins D, Wilschanski M. Maintenance of nutritional status in patients with cystic fibrosis: New and emerging therapies. Drug Des Devel Ther. 2012; 6: 151-61
COW’S MILK PROTEIN ALLERGY AND BREASTFEEDING pg 19
Magdalena Marciniak, BSc, PgCert
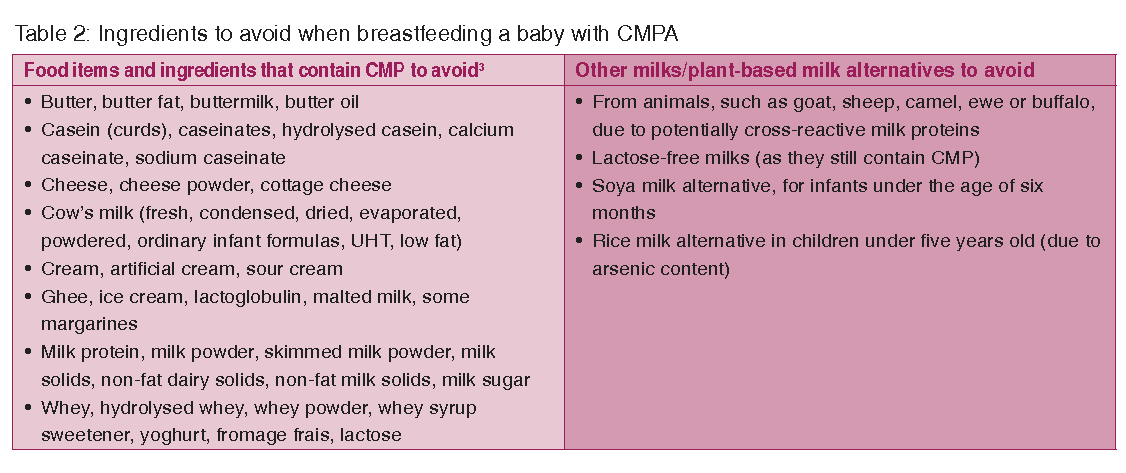
Table 2: Ingredients to avoid when breastfeeding a baby with cmpa SCOLL DOWN FOR TABLE 2
- Flom JD, Sicherer SH. Epidemiology of Cow's Milk Allergy. Nutrients. 2019; 11(5): 1051. Published 2019 May 10. doi:10.3390/nu11051051
- National Institute for Health and Clinical Excellence (NICE). Food allergy in children and young people. Diagnosis and assessment of food allergy in children and young people in primary care and community settings. Clinical guideline 116. February 2018. NICE. London
- Ludman S, Shah N, Fox AT. Managing cow’s milk allergy in children. BMJ. 2013; 347: f5424. Published 2013 Sep 16. doi:10.1136/bmj.f5424
- Martorell-Aragonés A, Echeverría-Zudaire L, Alonso-Lebrero E et al. Position document: IgE-mediated cow's milk allergy. Allergol Immunopathol (Madr). 2015; 43(5): 507-526. doi:10.1016/j.aller.2015.01.003
- Turnbull JL, Adams HN, Gorard DA. Review article: the diagnosis and management of food allergy and food intolerances. Aliment Pharmacol Ther. 2015; 41(1): 3-25. doi:10.1111/apt.12984
- Longo G, Berti I, Burks AW, Krauss B, Barbi E. IgE-mediated food allergy in children. Lancet. 2013; 382(9905): 1656-1664. doi:10.1016/S0140-6736(13)60309-8
- Vandenplas Y, Brueton M, Dupont C, Hill D, Isolauri E, Koletzko S, Oranje AP, Staiano A. Guidelines for the diagnosis and management of cow’s milk protein allergy in infants Arch Dis Child 2007; 92:902-908
- Host A, Halken S, Jacobsen HP, Christensen AE, Herskind AM, Plesner K. Clinical course of cow’s milk protein allergy/intolerance and atopic diseases in childhood. Allergy Immunol. 2002; 13:23-28. doi: 10.1034/j.1399-3038.13.s.15.7.x
- Luyt D, Ball H, Makwana N et al. BSACI guidelines for the diagnosis and management of cow’s milk allergy. Clinical & Experimental Allergy 2014 44, 642-672
- Venter C, Brown T, Meyer R et al (2017). Better recognition, diagnosis and management of non-IgE-mediated cow's milk allergy in infancy: iMAP – an international interpretation of the MAP (Milk Allergy in Primary Care) guideline. Clin Transl Allergy7(26), 1-9
- Fox A, Brown T, Walsh J et al. An update to the Milk Allergy in Primary Care guideline. Clin Transl Allergy. 2019; 9: 40. Published 2019 Aug 12. doi:10.1186/s13601-019-0281-8
- Fiocchi A, Brozek J et al. World Allergy Organisation (WAO) Diagnosis and rationale for action against cows milk allergy (DRACMA) guidelines. Pedatr Allergy Immunol 2010; 21; 1-125
- The GP infant feeding network (uk) (GPIFN). The Milk Allergy in Primary Care (MAP) Guideline2019. https://gpifn.org.uk/imap/
- Van Tulleken C. Overdiagnosis and industry influence: how cow’s milk protein allergy is extending the reach of infant formula manufacturers. BMJ 2018;363: 5056
- Department of Health (1991). Dietary reference values for food and energy and nutrients for the United Kingdom
- Adams J, Voutilainen H, Ullner PM, Järvinen KM. The safety of maternal elimination diets in breastfeeding mothers with food-allergic infants. Breastfeed Med. 2014; 9(10): 555-556. doi:10.1089/bfm.2014.0118
- Caffarelli C, Baldi F, Bendandi B et al. Cow's milk protein allergy in children: a practical guide. Ital J Pediatr. 2010; 36:5. Published 2010 Jan 15. doi:10.1186/1824-7288-36-5
- Henjum S, Lilleengen AM, Aakre I et al. Suboptimal Iodine Concentration in Breast milk and Inadequate Iodine Intake among Lactating Women in Norway. Nutrients. 2017; 9(7): 643. Published 2017 Jun 22. doi:10.3390/nu9070643
- Segal H, Meyer R, Shah N: JPGN. 2017: 64: 5. Published May 2017
- Bath SC, Hill S, Infante HG, Elghul S, Nezianya CJ, Rayman MP. Iodine concentration of milk-alternative drinks available in the UK in comparison with cow’s milk. Br J Nutr. 2017; 118(7): 525-532. doi:10.1017/S0007114517002136
- NIAID-Sponsored Expert Panel, Boyce JA, Assa'ad A et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010; 126(6 Suppl): S1-S58. doi:10.1016/j.jaci.2010.10.007
- Taylor-Black S, Wang J. The prevalence and characteristics of food allergy in urban minority children. Ann Allergy Asthma Immunol. 2012; 109(6): 431-437. doi:10.1016/j.anai.2012.09.012
- Grabenhenrich LB, Dölle S, Moneret-Vautrin A et al. Anaphylaxis in children and adolescents: The European Anaphylaxis Registry. J Allergy Clin Immunol. 2016; 137(4): 1128-1137.e1. doi:10.1016/j.jaci.2015.11.015
- Skypala IJ, Venter C, Meyer R et al. The development of a standardised diet history tool to support the diagnosis of food allergy. Clin Transl Allergy. 2015; 5:7. Published 2015 Feb 19. doi:10.1186/s13601-015-0050-2
Table 2: Ingredients to avoid when breastfeeding a baby with CMPA
CARING FOR OUR ELDERLY POPULATION: NUTRITIONAL CONSIDERATIONS AND BEYOND pg 25
Gaby Goodchild, RD
- https://www.who.int/health-topics/ageing
- https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021
- https://publichealthmatters.blog.gov.uk/2021/03/31/life-expectancy-in-england-in-2020/
- https://www.nhs.uk/live-well/eat-well/eight-tips-for-healthy-eating/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6316542/
- https://www.bda.uk.com/resource/osteoporosis-diet.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4337919/
- https://www.healthline.com/nutrition/nutritional-needs-and-aging
- https://www.bda.uk.com/resource/vitamin-d.html
- https://jnnp.bmj.com/content/74/7/959
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5130103/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4110863/
- https://www.nhs.uk/conditions/vitamin-b12-or-folate-deficiency-anaemia/symptoms/
- https://cks.nice.org.uk/topics/anaemia-b12-folate-deficiency/
- Nair KS. Aging muscle. Am J Clin Nutr. 2005; 81(5): 953-963
- https://pubmed.ncbi.nlm.nih.gov/15640517/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4924200
- Bauer J, Biolo G, Cederholm T et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. 2013; 14(8): 542-559
- https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/statistics-on-obesity-physical-activity-and-diet-england-2019/part-3-adult-obesity
- https://www.malnutritiontaskforce.org.uk/small-appetite/mental-health
- https://www.bda.uk.com/resource/malnutrition-in-older-people.html
- https://www.ageuk.org.uk/globalassets/age-uk/documents/reports-and-publications/reports-and-briefings/health--wellbeing/rb_feb13_understanding_the_oldest_old_improving_later_life.pdf
- https://www.helpguide.org/articles/depression/depression-in-older-adults.htm
- https://cks.nice.org.uk/topics/gastrointestinal-tract-lower-cancers-recognition-referral/
- https://cks.nice.org.uk/topics/constipation/management/adults/
- https://www.elder.org/the-elder/survey-on-elderly-loneliness/
NUTRITION IN CARE HOMES: FROM SCREENING TO ENTERAL FEEDING pg 31
Hazel Windsor-Aubrey, RD
- Edemekong PF, Bomgaars DL, Sukumaran S, Levy SB (2020). Activities of daily living. Available: https://www.ncbi.nlm.nih.gov/books/NBK470404/. Last accessed 12th May 2021
- Mlinac ME, Feng MC. Assessment of Activities of Daily Living, Self-Care, and Independence. Archives of Clinical Neuropsychology, Vol 31, Issue 6, September 2016, p 506-516
- Age UK (2018). New analysis shows number of older people with unmet care needs soars to record high Available: https://www.ageuk.org.uk/latest-press/articles/2018/july-2018/new-analysis-shows-number-of-older-people-with-unmet-care-needs-soars-to-record-high/. Last accessed 12th May 2021
- NHS (2019). Care homes. Available: https://www.nhs.uk/conditions/social-care-and-support-guide/care-services-equipment-and-care-homes/care-homes/. Last accessed 12th May 2021
- LaingBuisson (2020). Retirement housing: UK market report. Available: https://www.laingbuisson.com/wp-content/uploads/2021/01/LaingBuisson_Care_Homes_Older_People_31ed_CONTENTS.pdf. Last accessed 12th May 2021
- Wittenberg R, Hu B, Barraza-Araiza L, Rehill A (2019). Projections of older people with dementia and costs of dementia care in the United Kingdom, 2019-2040. The London School of Economics and Political Science. 5 (1), 1-79
- https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/january2021#:~:text=The%20UK's%20age%20structure%20is,trends%20in%20fertility%20and%20mortality.&text=By%202041%2C%20the%201960s%20baby,UK%2C%20compared%20with%202019%20figures. Accessed 12th May 2021
- Kingston A, Comas-Herreras A, Jagger C (2018). Forecasting the care needs of the older population in England over the next 20 years: estimates from the Population Ageing and Care Simulation (PACSim) modelling study. The Lancet. 3 (9), E447-E445
- Office for National Statistics (2018). Living longer: how our population is changing and why it matters. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongerhowourpopulationischangingandwhyitmatters/2018-08-13. Last accessed 12th May 2021
- Melzer D, Delgado JC, Winder R, Masoli J, Richards S, Ble A (2015). A reference on the frequency of major diseases, conditions and syndromes affecting older people in England. In: Ageing Research Group The Age UK almanac of disease profiles in later life. Exeter. 1-67
- Pout V (2014). Older Adults. In: Ageing Research Group Manual of Dietetic Practice. 5th ed. West Sussex: John Wiley and Sons LTD. 92-103
- Pilgrim AL, Robinson SM, Sayer AA, Roberts HC. An overview of appetite decline in older people. Nurs Older People. 2015; 27(5): 29-35
- World Health Organisation (2015). World Report on Ageing and Health. Available at: http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=1E50640D76C4D6C19D76446A528F0068?sequence=1. Last accessed 12th May 2021
- Cederholm T, Bosaeus I, Barazzoni R, Bauer J, Van Gossum A, Klek S, Muscaritoli M, Nyulasi I, Ockenga J, Schneider SM, de van der Schueren MA, Singer P. Diagnostic criteria for malnutrition – An ESPEN Consensus Statement. Clin Nutr. 2015 Jun; 34(3): 335-40
- BAPEN (2018). Malnutrition among Older People in the Community. Available: https://www.bapen.org.uk/resources-and-education/publications-and-reports/other-reports/malnutrition-among-older-people-in-the-community#:~:text=It%20affects%20over%2010%25%20of,over%20the%20age%20of%. Last accessed 12th May 2021
- McMahon K, Brown JK. Nutritional screening and assessment. Semin Oncol Nurs. 2000 May; 16(2): 106-12
- Elia M. The "MUST" report. Nutritional screening of adults: a multidisciplinary responsibility. Redditch, Worcs, UK: Malnutrition Advisory Group of the British Association for Parenteral and Enteral Nutrition, 2003.
- PENG: Parenteral and Enteral Nutrition Group (2018). A Pocket Guide to Clinical Nutrition. 5th ed. UK: British Dietetic Association . 3.16a
- Barkmeier JM, Trerotola SO, Wiebke EA, Sherman S, Harris VJ, Snidow JJ, Johnson MS, Rogers WJ, Zhou XH. Percutaneous radiologic, surgical endoscopic, and percutaneous endoscopic gastrostomy/gastrojejunostomy: comparative study and cost analysis. Cardiovasc Intervent Radiol. 1998 Jul-Aug; 21(4): 324-8
- Campoli P, Cardoso D, Turchi M, Mota O. Clinical trial: a randomised study comparing the durability of silicone and latex percutaneous endoscopic gastrostomy tubes. Dig Endosc. 2011 Apr; 23(2): 135-9
- Wireko BM and Bowling T (2010). Enteral tube feeding. Clinical medicine (London, England), 10(6), 616-619
IMD WATCH: CALL THE MIDWIFE… THEN, CALL THE DIETITIAN! pg 37
Suzanne Ford, RD
- Bickel H, Gerrard J, Hickmans EM (1953). Influence of phenylalanine intake on phenylketonuria. Lancet 265: 812-813
- Medical, Research and Council. Treatment of Phenylketonuria. Br Med J 1963, 1, 1691-1697
- Clayton B, Moncrieff A, Roberts E (1967). Dietetic Treatment of Phenylketonuria: a Follow-up Study. BMJ 15 July 1967
- Francis DE, Dixon DJ (1970). Diets for sick children (2nd ed)
- Ford S, O’Driscoll M, Macdonald A (2018). Living with Phenylketonuria: Lessons from the PKU community. Mol Genet Metab Rep. 2018, 17, 57-63
- Medford E, Hare DJ, Carpenter K, Rust S, Jones S, Wittkowski A (2017). Treatment Adherence and Psychological Wellbeing in Maternal Carers of Children with Phenylketonuria (PKU). In: Morava E, Baumgartner M, Patterson M, Rahman S, Zschocke J, Peters V (eds). JIMD Reports, Vol 37. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8904_2017_23
- Daly A, Evans S, Pinto A, Ashmore C, MacDonald A (2021). Protein Substitutes in PKU; Their Historical Evolution. Nutrients. 2021; 13(2): 484. https://doi.org/10.3390/nu13020484
- Guthrie R, Susa A (1963). A simple phenylalanine method for detecting phenylketonuria in large populations of newborn infants; Pediatrics Sep 1963, 32 (3) 338-343
CEREALS, WHOLEGRAINS AND NUTS p 41
Madi Myers, ANutr
- SACN (2015). Carbohydrates & Health. London: TSO
- Whole Grain Initiative (2020). Definition of a wholegrain food. Online. Available at: https://www.wholegraininitiative.org/media/attachments/2021/04/07/whole-grain-food-definition_v-2020-11-8-final.pdf
- National Diet and Nutrition Survey Years 1 to 9 of the Rolling Programme (2008/2009 – 2016/2017): Time trend and income analyses. https://www.gov.uk/government/statistics/ndns-time-trend-and-income-analyses-for-years-1-to-9. Jan 2019
- USDA (2020). Dietary Guidelines for Americans 2020-2025. Online. Available at: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- https://ec.europa.eu/jrc/en/health-knowledge-gateway/promotion-prevention/nutrition/food-based-dietary-guidelines
- Kromhout D et al (2016). The 2015 Dutch food-based dietary guidelines. Eur J Clin Nutr. 70(8): 869-878. doi: 10.1038/ejcn.2016.52
- Marshall S et al (2020). The Effect of Replacing Refined Grains with Whole Grains on Cardiovascular Risk Factors: A Systematic Review and Meta-Analysis of Randomised Controlled Trials with GRADE Clinical Recommendation. J Acad Nutr Diet. 120(11): 1859-1883.e31. doi: 10.1016/j.jand.2020.06.021
- Becerra-Tomás N et al (2019). Nut consumption and incidence of cardiovascular diseases and cardiovascular disease mortality: a meta-analysis of prospective cohort studies. Nutr Rev. 77(10): 691-709. doi: 10.1093/nutrit/nuz042
- de Souza RJ et al (2020). Association of nut intake with risk factors, cardiovascular disease and mortality in 16 countries from 5 continents: analysis from the Prospective Urban and Rural Epidemiology (PURE) study. Am J Clin Nutr. 112(1): 208-219. doi: 10.1093/ajcn/nqaa108
- Marventano S et al (2017). Whole Grain Intake and Glycaemic Control in Healthy Subjects: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Nutrients. 9(7): 769. doi: 10.3390/nu9070769
- Tindall AM et al (2019). The effect of nuts on markers of glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Am J Clin Nutr. 109(2): 297-314. doi: 10.1093/ajcn/nqy236
- Schlesinger S et al (2019). Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv Nutr. 10(2): 205-218. doi: 10.1093/advances/nmy092
- Sadeghi O et al (2020). Whole-Grain Consumption Does Not Affect Obesity Measures: An Updated Systematic Review and Meta-analysis of Randomised Clinical Trials. Adv Nutr. 11(2): 280-292. doi: 10.1093/advances/nmz076
- Akhlaghi M et al (2020). Effect of nuts on energy intake, hunger, and fullness, a systematic review and meta-analysis of randomised clinical trials. Crit Rev Food Sci Nutr. 60(1): 84-93. doi: 10.1080/10408398.2018.1514486
- Aune D et al (2011). Dietary fibre, whole grains, and risk of colorectal cancer: systematic review and dose-response meta-analysis of prospective studies. BMJ. 343: d6617. doi: 10.1136/bmj.d6617
- Zhang D et al (2020). Meta-analysis of the association between nut consumption and the risks of cancer incidence and cancer-specific mortality. Aging (Albany NY). 12(11): 10772-10794. doi: 10.18632/aging.103292
- Creedon AC et al (2020). Nuts and their Effect on Gut Microbiota, Gut Function and Symptoms in Adults: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Nutrients. 12(8): 2347. doi: 10.3390/nu12082347
- https://eatforum.org/eat-lancet-commission/
- https://www.bda.uk.com/resource/one-blue-dot.html
- Burlingame B, Dernini S, Nutrition and Consumer Protection Division, editor. Proceedings of the International Scientific Symposium: Biodiversity and Sustainable diets united against hunger 3-5 November 2010. Sustainable diets and biodiversity directions and solutions for policy, research and action. Rome: FAO; 2012. http://www.fao.org/docrep/016/i3004e/i3004e.pdf
IN COOKE’S CORNER pg 46
CGR Cooke, ANutr
- Youtube.com ((2016). The Allotment Project [online] Available at: <https://www.youtube.com/watch?v=mQxxpwCeD_U&ab_channel=CGRCooke> [Accessed 1 May 2021]
- Statista (2021). Coca-Cola Co: ad spend 2020 | Statista [online]. Available at: <https://www.statista.com/statistics/286526/coca-cola-advertising-spending-worldwide/> [Accessed 1 May 2021]
- The King's Fund (2021). Spending on public health [online]. Available at: <https://www.kingsfund.org.uk/projects/nhs-in-a-nutshell/spending-public-health#:~:text=In%202019%2F20%2C%20the%20value,authorities%20was%20%C2%A33.3%20billion.> [Accessed 1 May 2021]
- Gladwell M (2015). David and Goliath. Penguin
DIETETIC RESEARCH: HOW TO PUT TOGETHER A STUDY PROJECT pg 49
Barira Saad, RD
- Organising Your Social Sciences Research Paper. Detailed guidance on how to develop, organise, and write a college-level research paper in the social and behavioural sciences. Research guides. https://libguides.usc.edu/writingguide/researchproposal
- The KAP Survey Model (Knowledge, Attitudes and Practices). https://www.spring-nutrition.org/publications/tool-summaries/kap-survey-model-knowledge-attitudes-and-practices
- Hypotheses by Prof William MK Trochim. Research Methods Knowledge Base: https://conjointly.com/kb/hypotheses-explained/
- Barira Azfar, Muhammad Arif Khan, Ammar Ahmad Khan, Shaista Jabeen, Wajeeha Sultana, Aqsa Shafeeq, Mehtab Zahid, Fariha Azhar (2018). Assessment of Awareness Regarding the Advantages of Lactation Among Nursing Mothers in Lahore. https://bit.ly/3eW0V22