WEIGHT STIGMA: WHY BEING KIND IS KEY TO ADDRESSING OBESITY
Posted on
Weight stigmatisation is commonly regarded as the last form of acceptable discrimination, compared to sex, ethnicity and mental health. On a daily basis, people living with overweight and obesity have to face discrimination and it even lurks where we least expect it, says Beth Bradshaw, ANutr from the charity Food Active.
WHAT IS WEIGHT STIGMA?
Weight stigma refers to the discriminatory acts and ideologies targeted towards individuals because of their weight and size.1
WHERE CAN WEIGHT STIGMA BE FOUND?
Weight stigma, bias and discrimination can be found across different forms of communications in a wide range of contexts – most notably the media and in the workplace.
Sadly, children also report weight stigma in educational settings from teachers and peers, manifesting itself through verbal teasing/bullying, physical bullying or social exclusion from their peers due to their body weight.2
Arguably, most shockingly of all, however, is the evidence that suggests weight bias and stigmatisation is prevalent in healthcare settings, places in which we seek support, reassurance and guidance. Evidence suggests that some healthcare providers, including clinicians, nurses and dietitians, can hold strong negative attitudes and stereotypes about people with obesity, which can negatively influence person-perceptions, judgment, interpersonal behaviour and decision-making. All of which ultimately boils down to a lower quality of treatment and care for patients with obesity.3
Weight stigma is also present in public health messaging and campaigns, which can often describe obesity as a modifiable lifestyle behaviour – see the Cancer Research UK’s ‘OB_S_ _Y’ campaign in 2019 (Figure 1).
FIGURE 1: Cancer Research UK Obesity and Cancer Awareness Campaign. Image from CRUK Campaign Imagery.
WHAT ARE THE MAIN ISSUES WITH WEIGHT STIGMA?
- It is unkind. It can lead to those living with overweight and obesity having low self-esteem and depression. It can lead to social rejection by peers and other individuals.4 In a world where we can be anything, we should be kind – to everyone, regardless of their weight.
- It is completely unjust. We know that our weight is influenced by a wide range of different factors, not just what we choose as an individual: where we are born, where we work, our household income, the amount of marketing we are exposed to, our access to local green spaces, our genetics – the list goes on.5 So why is obesity viewed as simply an individual choice? Or simply a modifiable lifestyle factor? With the majority of adults in England now living with overweight or obesity,6 it is high time we stopped blaming the individual.
- It can also have negative physical impacts, such as creating an unhealthy relationship with food, which could in turn lead to reinforced weight gain. In the context of addressing obesity, it is clear that weight stigma is hindering efforts to address obesity. Is it any wonder there has been little to no success in reducing obesity in England when weight stigma is so prevalent?
HOW CAN ELIMINATING WEIGHT STIGMA HELP TO ADDRESS OBESITY?
There are significant benefits to stamping out weight stigma on efforts to reduce the prevalence of obesity. By ensuring healthcare providers are compassionate, understanding and knowledgeable about the complexities of preventing and treating obesity, people with obesity would be more likely to access care to support them in treating their condition and ultimately lose weight.
The government would also be more likely to place the focus on addressing the wider determinants and structural drivers of obesity (through implanting national policy on the food environment and tackling food poverty and food insecurity, for example). Better this than viewing obesity as simply a modifiable health behaviour and investing millions of pounds into social marketing campaigns, such as the current ‘Better Health: Let’s Do This’ campaign, which, despite being designed to reduce obesity, can unintentionally be complicit in contributing to weight stigma through conveying the narrative that losing weight is as simple as ‘eat well, move more’.
WHAT CAN I DO?
We can all do our bit to help eliminate weight stigma – and whilst it can sometimes be done unknowingly, it is important to ensure our own communications around obesity are free from stigmatisation for people living with obesity.
Earlier this month, at Food Active, we marked World Obesity Day by publishing a new resource to help support stigma-free communications across a wide range of platforms.7 Please do have a read – but in the meantime, some of the simple and easy ways we can all help to end weight stigma include:
Use non-stigmatising language when communicating about obesity. This includes using people-first language that emphasises the individual, not the disability / disease.
FIGURE 2: Food Active Weight Stigma Checklist (2021)
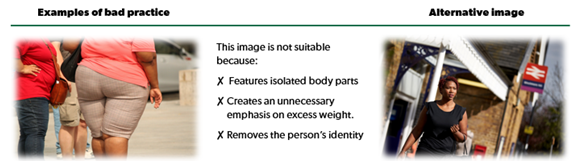
Use non-stigmatising images of people with obesity. Such images are free to download from the World Obesity Image Bank, the Rudd Center Media Gallery and others.
FIGURE 3: Food Active Weight Stigma Checklist (2021) – left image by Anja from Pixabay and right image from World Obesity Federation.
And finally, #BeKind. To anyone and everyone – regardless of their weight.
Beth Molly Bradshaw, ANutr
Food Active, Health Equalities Group
Beth has a passion for the wider determinants of health
and campaigning for an environment that is more conducive
to healthy lifestyles and behaviours. She has worked at Food Active,
a healthy weight charity, since 2017 and volunteered for a further 18 months.
Beth has an undergraduate and master’s degree in food, nutrition and public health.
Twitter: @BMBradshaw95
LinkedIn: @BethBradshaw1995
Email: [email protected]
References
- World Obesity Federation. Weight stigma: https://www.worldobesity.org/what-we-do/our-policy-priorities/weight-stigma [Accessed: 16th March 2021]
- Nutter, S., Ireland, A., Alberga, A.S. et al. (2019) Weight Bias in Educational Settings: a Systematic Review. Curr Obes Rep 8, 185–200.
- Phelan, S.M., Burgess, D.J., Yeazel, M.W., Hellerstedt, W.L., Griffin, J.M. and Ryn, M van. (2015) Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Reviews. 16 (4), 319-326.
- Emmer, C, Bosnjak, M, Mata, J. The association between weight stigma and mental health: A meta‐analysis. Obesity Reviews. 2020; 21: 12935.
- Government Office for Science (2007) Foresight: Tackling obesities – future choices. Project Report (2nd ed). https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf [Accessed: 22nd March 2021].
- NHS England (2020) Statistics on Obesity, Physical Activity and Diet, England, 2020. https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-obesity-physical-activity-and-diet/england-2020/part-3-adult-obesity-copy [Accessed: 22nd March 2021]
- Food Active (2021) Stamping out weight stigma: a checklist for the workforce [online] Available at: https://foodactive.org.uk/wp-content/uploads/2021/03/Weight_Stigma_Checklist_FoodActive_FINAL.pdf [Accessed: 22nd March 2021]
